The Bottom Line:
- Low joint fluid affects all ages and health levels
- Low joint fluid can not only cause pain or stiffness, but affect your mobility and potentially damage cartilage
Have you ever exercised hard and ended up with a sore knee the next day? Or have you experienced swelling and pain in your joints seemingly without reason?
You may have synovitis or low joint fluid. How do you know if it’s an injury or something more? Can you treat it?
Fortunately, you can not only diagnose and treat synovitis, but you can also prevent it too.
What Causes Low Joint Fluid
There are a few reasons why one might suffer from low joint fluid or synovium. It’s not something that discriminates with age or health.
Many healthy people can also suffer from this issue. However, it’s generally a condition that’s not primary.
Sometimes it’s caused by something as simple as an injury to the joint or as serious as cancer.
For those that are healthy, it’s primarily caused by overuse of the joint. For example, if you’re an athlete or work a job that requires you to lift or squat, you may have joint issues.
However, it is more prone to those that aren’t healthy. People who have inflammatory arthritis often suffer from an overgrowth of the synovium.
This is an abnormal immune response, and the body ends up misidentifying the natural cartilage and attacks it.
The loss of cartilage damages the surface of the joint and can lead to stiffness and pain found in all types of arthritis.
The most common type of arthritis, osteoarthritis, doesn’t have an inflammatory response.
Other types of joint conditions like gout, bleeding disorders, and infections can change the way your joint fluid looks and feels.
The low joint fluid doesn’t just cause pain or stiffness. It can affect your mobility and cause damage to your cartilage.
Some conditions synovitis has been linked to include:
- Injury
- Overuse
- Poor support
- Juvenile arthritis
- Gout
- Rheumatoid arthritis
- Osteoarthritis
- Rheumatic fever
- Psoriatic arthritis
- Cancer
- Lupus
- Infections
- Tuberculosis
What Is Synovitis?
Synovitis occurs when the synovium of a joint becomes inflamed or swollen. Your joints are encased in connective tissue inside the joint capsule.
This connective tissue is called the stratum synoviale or synovial stratum.
The joint capsule (the articular capsule) surrounds joints like the shoulder, wrist, elbow, hand, knee, foot, and ankle.
It has a tough outer layer called the fibrous stratum and a soft inside layer called the synovium.
Contained in both layers lies the synovial fluid. This fluid is viscous and lubricates the joints to protect them and reduce friction when you perform a movement.
Types of Synovitis
As it was mentioned earlier, anyone can suffer from joint problems, even children. Children often suffer from transient synovitis.
Transient synovitis typically happens after a child has experienced a viral infection. The virus settles in the fluid that surrounds the joints.
This can cause joint pain, limping, or in some cases immobility. The symptoms can appear and reappear suddenly and change places.
This condition often puts people in a panic because you develop a low-grade fever or none but suddenly have pain and can’t walk.
For some reason, this condition occurs in boys twice as often as girls. It also affects the right side of the body.
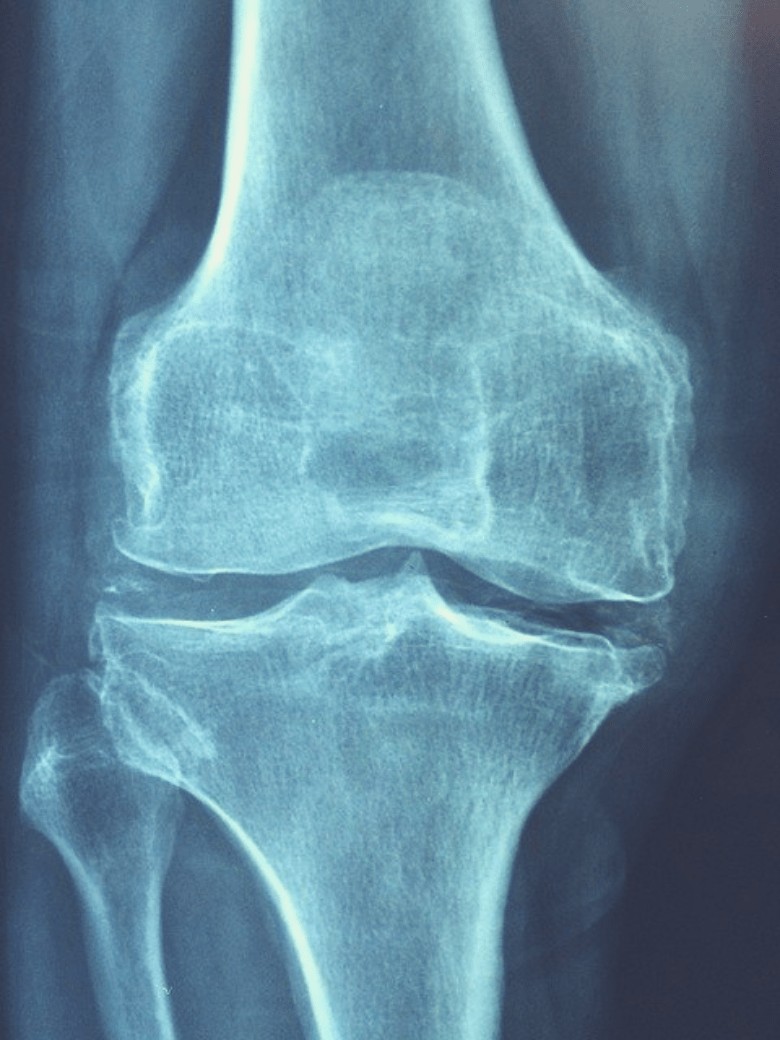
The only way to test for transient synovitis is from X-rays. Other tests rule out more severe types of synovitis like septic synovitis, and other conditions like arthritis and injuries.
The good news is that transient synovitis clears within a week or two, and patients don’t suffer from long-term side effects.
It’s recommended that if your child alerts you to joint pain or immobility, to seek a specialist or pediatrician.
Chronic synovitis is often referred to as “water on the knee.” It’s inflammation that reoccurs after an acute synovitis episode.
Post-traumatic synovitis occurs from overuse or injury to the joint. Your movements combined with weight-bearing causes the synovium to inflame.
This adds to the risk of further injury and causes pain, swelling, tenderness, and immobility of the joint.
The most severe type of synovitis is called pigmented villonodular synovitis or PVNS. This type affects the knee and hip joints.
However, this condition causes the synovial membrane to grow into a benign tumor. Your joints can lock up while you try to move or walk.
It starts with slow or rapid swelling and that happens suddenly but comes and goes. It’s important that you seek medical attention immediately and not self-treat this condition.
Despite the severity, this type of synovitis is very rare.

Symptoms
There are two sets of symptoms for synovitis: subclinical and active. Subclinical synovitis inflamed the lining of the joint and isn’t detectable during an initial physical exam.
This type of synovitis is found through an MRI or ultrasound.
Active synovitis refers to the inflammation, warmth, or redness that’s visible during a physical exam.
When synovitis gets to the point where it’s observable during an exam, permanent joint damage becomes the concern.
The main symptom of synovitis is joint pain. The pain is often more severe than thought because there’s no outward damage or appearance that it’s damaged.
You may not have swelling or any signs of injury except for pain. Some may have swelling, warmth, redness, or difficulty moving the joint.
You may have “popping” or “clicking” sensations in your joint when you move it or pressure.
Some people develop nodules or hard lumps around the affected area. Your joint might have dysfunction or cartilage erosion.
This can lead to osteoarthritis.
Symptoms that aren’t outwardly noticed are thickening of the tissue, increased blood flow to the area, and increased fluid production.
How to Diagnose and Treat Synovitis
Before you begin a treatment plan, you’ve to get diagnosed with a low joint fluid issue. When you go to a doctor or specialist, they’ll perform a physical exam first.
Then, they’ll order a synovial fluid analysis. Synovial fluid analysis is a series of tests that checks for medical issues that can affect the joints.
Usually, there are three types of tests conducted. The first test involves an exam of the fluid to check its color and thickness.
The second test uses chemicals to see the changes in the fluid’s chemical makeup. The third test uses microscopes to look for bacteria, foreign substances, or crystals.
A synovial fluid analysis could determine if you have osteoarthritis, gout, rheumatoid arthritis, joint effusion, joint infection, or bleeding disorder.
Test for Synovitis
When you need a fluid analysis, your doctor will numb the area (joint) with a local anesthetic. They will put a needle in the area and take a sample of fluid.
No set amount of fluid’s taken from you until it’s determined how many tests you’ll need or how big the joint is.
Your sample goes to the lab where a technician takes a closer look at it. Your fluid will undergo an examination of various changes.
These changes include:
- A change in color or thickness
- Proteins, uric acid, and glucose
- Lactic dehydrogenase (an enzyme that can increase inflammation)
- Crystals
- Your red and white blood cells
- Bacteria, viruses, and foreign substances
To determine if you have abnormal synovial fluid, your results will show a few issues. However, first, we will discuss what normal synovial fluid looks like.
Normal synovial fluid looks clear or pale yellow, stringy, and free of bacteria or foreign substances. Abnormal results will show various fluid changes. These changes include:
- Cloudy or thick fluid.
- High uric acid or crystals could indicate gout.
- A high white blood cell count could indicate an infection or medical problem.
- A high red blood cell count could indicate an injury, blood in the joint, or bleeding disorders.
- Lactic dehydrogenase
You may also have to undergo other tests if your doctor or specialist thinks your joint issues stem from another problem.
Your doctor might want to determine where the source of your pain is and if it’s from inside the joint (synovitis) or inflamed tendons (tendonitis).
You may have to undergo an MRI or an ultrasound of your musculoskeletal problem areas.
Treatment
There are a few ways to treat synovitis. However, there is no cure. The current treatments range from drugs to a procedure.
Many patients that have this disorder take anti-inflammatory medicines and rest.
These oral drugs could include steroids or DMARDs (disease-modifying antirheumatic drugs). In severe cases, you might have to take steroid injections.
Physical therapy complimentary to drug therapy may help too.
Some patients opt for physical therapy to help strengthen their joints and muscles, reduce pain, and prevent motion loss in the affected joint.
Some patients don’t respond well to either of these treatments. If they don’t, you may have to see an orthopedic surgeon for a procedure called a synovectomy.
This procedure removes most of your synovium. This can relieve pain, stiffness, and in some cases restore mobility.
Some may need further inventions like radionuclide synovectomy or arthroscopic synovectomy.
A radionuclide synovectomy may be considered invasive. It requires a radioactive substance to be injected into the affected joint.
This low-level radiation melts the inflamed synovium away. Many patients have concerns with this treatment because of the radiation.
A surgical intervention called arthroscopic synovectomy can help relieve symptoms and issues but is often used when damage to the joint is already present.
This surgery removes the inflamed part of the synovial membrane.
Unfortunately, this surgery can’t help restore your range of motion or improve it. But it can help with further joint damage and bleeding.
Prevention of Synovium
There are some ways you can prevent synovium. One obvious reason, if you’re a healthy person, is to ensure you get the proper amount of rest needed in between workouts.
Also, take proper care in recovery times. If you can, try to avoid stress on the joints like running.
Exercise isn’t something that you should avoid. But when you work out, you want to partake in certain exercises.
Strengthening exercises will help support your muscles, tendons, and ligaments. Along with your workouts, you want the right type of shoes.
Your shoes should have cushioning at the heel or orthotic inserts.
Your diet can help with prevention too. Stay hydrated and drink the recommended eight cups of water a day (or more depending on how active you are).
Proper hydration will help your body function.
You want to make sure your diet doesn’t contain a bunch of junk or unhealthy foods. Diets rich in protein will help your muscles grow stronger and recover faster.
Foods that contain anti-inflammatory properties like fruits and dark leafy vegetables can help with the swelling of the joints.
They’re also rich in antioxidants that help with synovial fluid levels. Nuts, seeds, and protein high in omega-3s help keep the joints healthy and your fluid healthy too.
Foods high in allicin (garlic, onions, fermented foods) don’t just help your digestive system. They aid in your joint’s health.
While these are not guaranteed to totally prevent synovitis. They can help reduce your risk of developing it.
Final Thoughts
Joint issues can affect anyone regardless of their age. Some of these issues are relieved by rest, but others may require further medical intervention.
However, you don’t have to suffer from joint pain or immobility. There are ways you can treat your low joint fluid or synovitis, should you have it.
Most of the treatments are invasive and could help restore your movement or just relieve the pain you feel on an everyday basis.